PORTAL runs a monthly seminar series that convenes two experts from different fields or vantage points to discuss how various aspects of therapeutic development and use are affected by ethical norms, laws, and regulations. These are organized in conjunction with the HMS Center for Bioethics supported by the Oswald DeN. Cammann Fund at Harvard University.
You may join the discussion on Twitter before, during, or after each event by following @PORTAL_Research and using the hashtag #policyethx.
You may join the discussion on Twitter before, during, or after each event by following @PORTAL_Research and using the hashtag #policyethx.
Health Policy & Bioethics Consortia 2016-2017
Private Investment vs. Public Funding in Therapeutic Development
May 12, 2017 | Harvard Medical School
There is substantial controversy around the contributions of different sectors in the biomedical research community towards the creation of highly innovative products. Emerging research has also pointed to the valuable, yet under-recognized, role played by public investment. By contrast, the pharmaceutical industry has long contended that it is responsible for most new medicines. In recent years, some large academic centers have actively sought out private funding, including venture capitalists, in supporting their research. What are the implications of different economic models of funding biomedical sciences for the types of products that emerge, and for the ultimate goal of improving patient care options?
May 12, 2017 | Harvard Medical School
There is substantial controversy around the contributions of different sectors in the biomedical research community towards the creation of highly innovative products. Emerging research has also pointed to the valuable, yet under-recognized, role played by public investment. By contrast, the pharmaceutical industry has long contended that it is responsible for most new medicines. In recent years, some large academic centers have actively sought out private funding, including venture capitalists, in supporting their research. What are the implications of different economic models of funding biomedical sciences for the types of products that emerge, and for the ultimate goal of improving patient care options?
|
EXPERTS:
Terry McGuire, MS, MBA Founding Partner, Polaris Partners Bhaven Sampat, PhD Professor of Health Policy and Management Columbia University Mailman School of Public Health MODERATOR: Ariel D. Stern, MA, PhD Assistant Professor of Business Administration Technology and Operations Management Unit Harvard Business School |
Medical Errors and the Culture of Medicine
April 14, 2017 | Harvard Medical School
With decades of experience behind the patient safety movement, we now have a clear understanding of the importance of preventing medical errors. However, progress in this area has been mixed, with the field still struggling with fundamental questions: how reliably can we identify errors and determine whether a death was preventable? Does this heightened focus on patient safety further the perception that death is most often the result of mistakes that can be avoided? And how can we most effectively scrutinize our practices and improve outcomes?
April 14, 2017 | Harvard Medical School
With decades of experience behind the patient safety movement, we now have a clear understanding of the importance of preventing medical errors. However, progress in this area has been mixed, with the field still struggling with fundamental questions: how reliably can we identify errors and determine whether a death was preventable? Does this heightened focus on patient safety further the perception that death is most often the result of mistakes that can be avoided? And how can we most effectively scrutinize our practices and improve outcomes?
|
EXPERTS:
Timothy Hofer, MD Professor of Internal Medicine Associate Director for Analytic and Information Resources University of Michigan Martin Makary, MD, MPH Professor of Surgery Johns Hopkins University School of Medicine Professor of Health Policy & Management Johns Hopkins Bloomberg School of Public Health MODERATOR: Chana Sacks, MD HMS General Internal Medicine fellow |
Promoting Accurate and Useful Public Reporting on Physicians
March 29, 2017 | Harvard Medical School
Public reporting has been proposed as a tool for improving the transparency and quality of health care delivery. Hospitals now dedicate substantial resources towards reporting requirements for measures such as mortality for selected conditions (e.g. pneumonia, heart failure) and outcomes of cardiac procedures. However, the enormous effort and expense supporting public reporting have raised questions about whether such programs actually improve public health, or may even be misleading or harmful. For example, risk adjustment tools may lack the refinement necessary to yield sound results, forcing a delicate balance between providing more information to the public with only limited context. Also, there may be potential unintended consequences of public reporting, such as adverse selection, that may actually worsen clinical outcomes. What, ultimately, are the ways in which public reporting can be shaped to improve quality of care, transparency, and outcomes?
March 29, 2017 | Harvard Medical School
Public reporting has been proposed as a tool for improving the transparency and quality of health care delivery. Hospitals now dedicate substantial resources towards reporting requirements for measures such as mortality for selected conditions (e.g. pneumonia, heart failure) and outcomes of cardiac procedures. However, the enormous effort and expense supporting public reporting have raised questions about whether such programs actually improve public health, or may even be misleading or harmful. For example, risk adjustment tools may lack the refinement necessary to yield sound results, forcing a delicate balance between providing more information to the public with only limited context. Also, there may be potential unintended consequences of public reporting, such as adverse selection, that may actually worsen clinical outcomes. What, ultimately, are the ways in which public reporting can be shaped to improve quality of care, transparency, and outcomes?
|
EXPERTS:
Robert Yeh, MD, MBA Director, Richard and Susan Smith Center for Outcomes Research in Cardiology Beth Israel Deaconess Medical Center and Harvard Medical School Thomas Lee, MD Chief Medical Officer Press Ganey MODERATOR: Daniel B. Kramer, MD Assistant Professor of Medicine, HMS & Cardiac Electrophysiologist, Div. of Cardiovascular Medicine & the Cardiovascular Institute, Beth Israel Deaconess Medical Center |
Returning Results to Research Participants
February 10, 2017 | Harvard Law School
Clinical investigators, public health advocates, and institutional review boards have been struggling to develop appropriate policies on how to return results to patients involved in research studies. These results may come in a variety of forms, ranging from aggregated study results to individual results to incidental findings. Experts disagree over the optimal timing, how researchers should consider the burden that these results can place on patients, and whether there are circumstances in which certain findings should be withheld. Is clinical utility the appropriate standard, or does mere curiosity suffice to trigger disclosure obligations? How certain must the results be, and what if there is reason to believe that the results will be difficult for participants to understand – or cause them harm? Two experts in the field of research law and ethics will join us to engage these and other questions, and help conceive a way to move forward in the best interests of patients and the medical research enterprise.
Clinical investigators, public health advocates, and institutional review boards have been struggling to develop appropriate policies on how to return results to patients involved in research studies. These results may come in a variety of forms, ranging from aggregated study results to individual results to incidental findings. Experts disagree over the optimal timing, how researchers should consider the burden that these results can place on patients, and whether there are circumstances in which certain findings should be withheld. Is clinical utility the appropriate standard, or does mere curiosity suffice to trigger disclosure obligations? How certain must the results be, and what if there is reason to believe that the results will be difficult for participants to understand – or cause them harm? Two experts in the field of research law and ethics will join us to engage these and other questions, and help conceive a way to move forward in the best interests of patients and the medical research enterprise.
|
EXPERTS:
Barbara Bierer, MD Program Director, Regulatory Foundations, Law and Ethics Program, Harvard Catalyst Faculty co-director, Multi-Regional Clinical Trials (MRCT) Center of Brigham and Women's Hospital and Harvard Medical School Pilar Ossorio, JD, PhD Professor of Law and Bioethics University of Wisconsin Law School MODERATOR:
Holly Lynch, JD, MBioethics Executive Director, Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics Harvard Law School |
|
Clinical Trial Data Sharing and Reproducibility
December 7, 2016 | Harvard Medical School
In January, the International Committee of Medical Journal Editors proposed requiring investigators make de-identified trial data available six months after publication as a precondition of consideration. Many data scientists support the policy and champion even more stringent standards as a means to accelerate scientific advances, tackle the problem of irreproducibility, and fulfill moral obligations to research participants. However, numerous trialists have raised potential challenges in the push toward greater data sharing, including researchers analyzing data with which they are not intimately familiar, diminished incentives for primary data collection, and shared data usability.
The ongoing debate has exposed a number of important questions regarding the ownership of publicly and privately funded trial data, the ethical duties of society and researchers to trial participants, and the possible benefits and harm of rapid widespread data sharing.
In January, the International Committee of Medical Journal Editors proposed requiring investigators make de-identified trial data available six months after publication as a precondition of consideration. Many data scientists support the policy and champion even more stringent standards as a means to accelerate scientific advances, tackle the problem of irreproducibility, and fulfill moral obligations to research participants. However, numerous trialists have raised potential challenges in the push toward greater data sharing, including researchers analyzing data with which they are not intimately familiar, diminished incentives for primary data collection, and shared data usability.
The ongoing debate has exposed a number of important questions regarding the ownership of publicly and privately funded trial data, the ethical duties of society and researchers to trial participants, and the possible benefits and harm of rapid widespread data sharing.
|
|
EXPERTS:
Jeff Drazen, MD Editor-In-Chief, New England Journal of Medicine Distinguished Parker B. Francis Professor of Medicine, Harvard Medical School Harlan Krumholz, MD, SM Harold H. Hines, Jr. Professor of Medicine (Cardiology) Director, Center for Outcomes Research and Evaluation, Yale-New Haven Hospital MODERATOR: Ameet Sarpatwari, JD, PhD Assistant Director, Program on Regulation, Therapeutics, and Law (PORTAL) Instructor of Medicine, Harvard Medical School |
The Hope and Hype of Precision Medicine
November 16, 2016 | Harvard Medical School
There has been considerable hype surrounding personalized and precision medicine in the past few years—including President Obama’s 2015 announcement of $215 million for the Precision Medicine Initiative. While some policymakers hail this movement as a pending revolution in healthcare, other commentators are skeptical, arguing that the same funding directed toward the social and behavioral determinants of health would yield far greater gains in terms of patient benefits and healthcare savings.
How important is precision medicine for our healthcare marketplace, and what should the expected outcomes be for public investment in research in this area?
There has been considerable hype surrounding personalized and precision medicine in the past few years—including President Obama’s 2015 announcement of $215 million for the Precision Medicine Initiative. While some policymakers hail this movement as a pending revolution in healthcare, other commentators are skeptical, arguing that the same funding directed toward the social and behavioral determinants of health would yield far greater gains in terms of patient benefits and healthcare savings.
How important is precision medicine for our healthcare marketplace, and what should the expected outcomes be for public investment in research in this area?
|
EXPERTS:
Sandro Galea, MD, MPH, DrPH Dean and Robert A. Knox Professor Boston University School of Public Health Calum A. MacRae, MD, PhD Chief of Cardiovascular Medicine and Associate Professor Brigham & Women’s Hospital and Harvard Medical School MODERATOR:
Spencer Hey, PhD Faculty, Harvard Medical School Center for Bioethics Research Fellow, PORTAL |
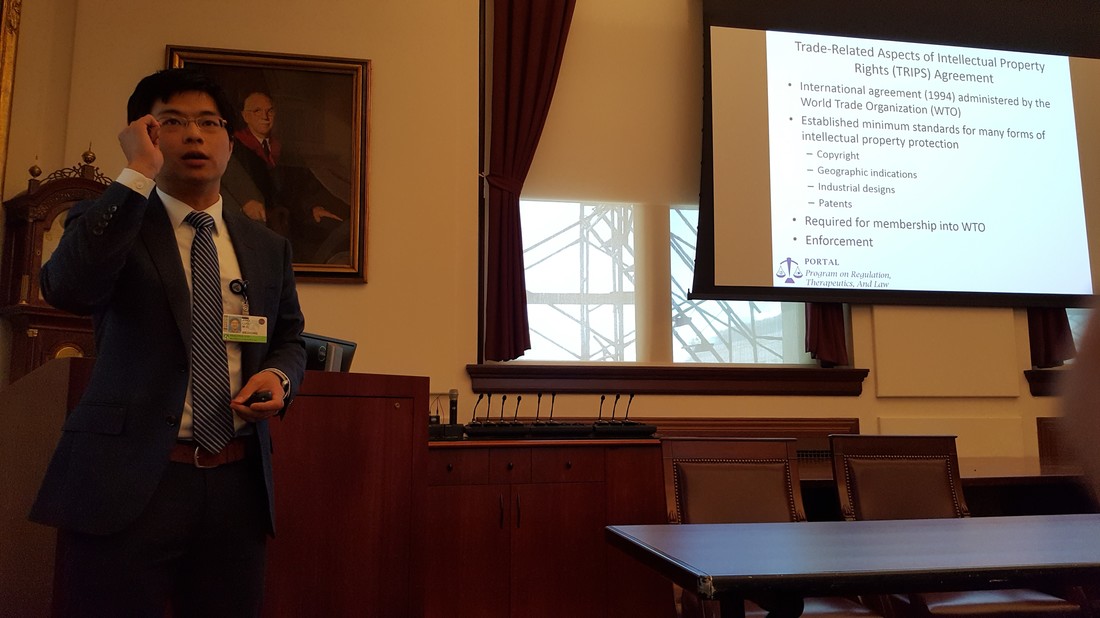
International Trade and Access to Medicines
October 14, 2016 | Harvard Medical School
The Trans-Pacific Partnership (TPP) Agreement is intended to facilitate trade among 12 Asia-Pacific countries including the US, but its progress has been obstructed in part by ongoing controversy over provisions regarding intellectual property protections for pharmaceutical products. Some argue that if signed, the TPP will impact the availability or cost of essential medicines in low-income settings worldwide by requiring all countries to provide high levels of IP protections mirroring current US standards. Join us as we discuss the implications of the TPP for US patients (and patents), and the proper role of public health concerns in international trade negotiations.
The Trans-Pacific Partnership (TPP) Agreement is intended to facilitate trade among 12 Asia-Pacific countries including the US, but its progress has been obstructed in part by ongoing controversy over provisions regarding intellectual property protections for pharmaceutical products. Some argue that if signed, the TPP will impact the availability or cost of essential medicines in low-income settings worldwide by requiring all countries to provide high levels of IP protections mirroring current US standards. Join us as we discuss the implications of the TPP for US patients (and patents), and the proper role of public health concerns in international trade negotiations.
The Ethical Involvement of Patients in FDA Regulatory Evaluation of New Products
September 9, 2016 | Harvard Medical School
There is a growing push to incorporate patient voices more directly at the FDA in decisionmaking about investigational drugs, but what are the optimal parameters of patients' contributions?
There is a growing push to incorporate patient voices more directly at the FDA in decisionmaking about investigational drugs, but what are the optimal parameters of patients' contributions?
- How should individual patient voices be weighed against the accumulated data about a drug?
- Can we better educate patients to equip them to engage in discussions about trial design, statistics, and evaluation?
- How should we consider financial relationships between patient advocacy groups and the pharmaceutical industry sponsor of a drug?
|
EXPERTS:
Walid Gellad, MD, MPH University of Pittsburgh, VA Medical Center Diana Zuckerman, PhD National Center for Health Research MODERATOR:
Aaron S. Kesselheim, MD, JD, MPH Brigham and Women’s Hospital and Harvard Medical School |
|
|
Program On Regulation, Therapeutics And Law (PORTAL)
Division of Pharmacoepidemiology and Pharmacoeconomics 1620 Tremont Street, Suite 3030 Boston, MA 02120 |